-
Abuse-Deterrent Opioids and the Economic Costs of Abuse
How can industry participants help curb opioid abuse while maintaining appropriate access to care for patients?
Prescription opioid medications can be effective for patients suffering from painful conditions. At the same time, prescription opioid abuse – including dependence, overdose, and poisoning – has become a national public health concern.
Beyond the human toll of the increasing number of deaths traceable to abuse, prescription opioid abuse comes with considerable economic burden. Analysis Group’s research shows that prescription opioid abuse is associated with sharp increases in health care costs and medical resource utilization, as well as with higher caregiver burden, substantial workplace costs (lost earnings, medically related absenteeism, and disability claims), and criminal justice costs.
Recently, we examined the excess health care costs of opioid abuse – that is, costs documented for diagnosed abusers, beyond those found for a similar control group of patients who were not diagnosed as abusers. (See figure.) Excess costs begin accumulating well before the abuse diagnosis, spike during the incident diagnosis month, and remain elevated for 18 months following diagnosis. Prior to and including the diagnosis, a larger proportion of excess costs is incurred by use of emergency departments and inpatient services, perhaps indicating that acute abuse-related events lead to formal abuse diagnoses. Following diagnosis, maintenance care costs (outpatient services and rehabilitation facilities) tend to be higher, suggesting that diagnosed abusers continue to receive treatment in less-intensive forms.
Policy interventions such as Suspicious Order Monitoring programs are intended to help identify potential abuse earlier. Additionally, some pharmaceutical manufacturers have developed abuse-deterrent opioids (ADOs) – that is, opioids with properties intended to reduce the risk of abuse. The US Food and Drug Administration (FDA) has approved a number of these in the past several years.
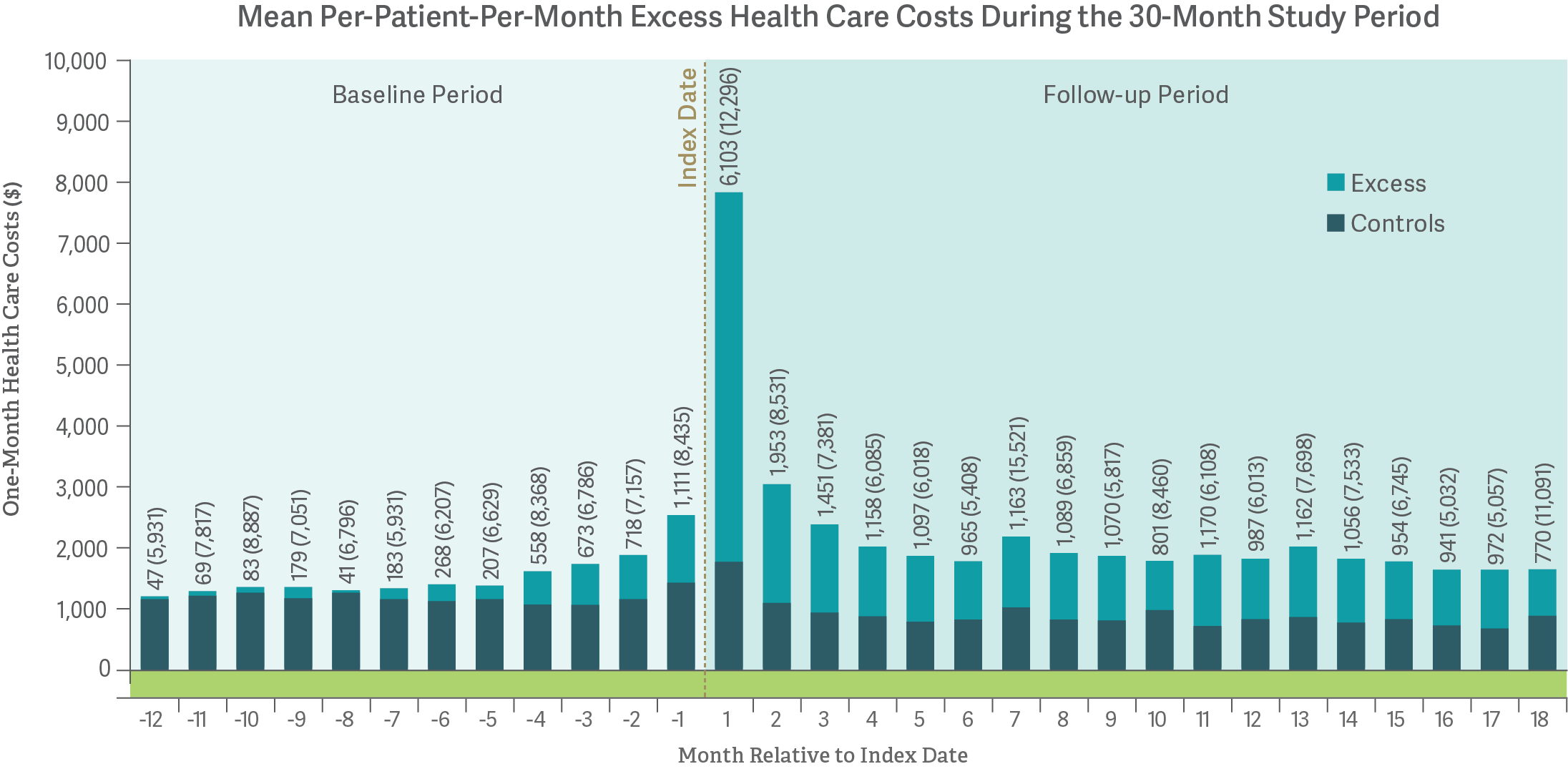
Notes: Mean monthly costs after diagnosis exclude patients in months for which they no longer have continuous eligibility. Standard deviations are shown in parentheses in the "Controls & Excess" display.
Recent results from our work suggest that ADOs may indeed hold the potential to reduce real-world abuse and total costs to the health care system. However, our studies have also raised the possibility that some patients may avoid treatment with ADOs when they become available, and that those who do are more likely to be abusers. This may be an unintended consequence of introducing ADOs in a therapeutic landscape that still includes both opioids without abuse-deterrent properties and illicit substances such as heroin.
These findings suggest that ADOs are part of a larger set of policy tools and should be considered along with additional initiatives, such as greater education of physicians, increased access to substance use treatment, and more rigorous identification and monitoring to identify patients at high risk of abuse. ■
Noam Y. Kirson, Managing Principal
Howard G. Birnbaum, Senior Advisor
Alan G. White, Managing PrincipalSources: “Use of prescription opioids with abuse-deterrent technology to address opioid abuse,” Edward Michna, Noam Y. Kirson, Amie Shei, Howard G. Birnbaum, Rami Ben-Joseph, Current Medical Research and Opinion, 30:8, 1589-1598 (2014); “Drivers of Excess Costs of Opioid Abuse Among a Commercially Insured Population,” Lauren M. Scarpati, Noam Y. Kirson, Miriam L. Zichlin, Zitong B. Jia, Howard G. Birnbaum, Jaren C. Howard, American Journal of Managed Care, May 22, 2017; “Opioid Abuse: A Detailed Examination of Cost Drivers over a 24-Month Follow-up Period,” Lauren M. Scarpati, Noam Y. Kirson, Zitong B. Jia, Jody Wen, Jaren Howard, Journal of Managed Care & Specialty Pharmacy, June 6, 2017; “A Harm Reduction Model to Quantify Potential Misuse/Abuse Reduction and Abuse-Related Events Avoided from Abuse Deterrent Opioids,” Alan White, Tim Spittle, Gwendolyn Niebler, Jeffrey Dayno, Colville Brown, Nathaniel Katz, presented at PAINweek 2017, September 7, 2017.