-
Educating Providers on Diagnostic Tools Could Improve Alzheimer’s Care Across Sociodemographic Groups
Certain tests to diagnose patients with mild cognitive impairment and mild dementia could support improvements in Alzheimer’s care, if providers know when to initiate them.
Alzheimer’s is not always recognized in individual patients at the earliest stages of the condition. Diagnostic tools such as neurocognitive assessments, biomarker tests, and other tools such as structural imaging to assess other potential causes of symptoms could help providers identify and treat patients with early Alzheimer’s disease (that is, those with mild cognitive impairment and mild dementia due to Alzheimer’s).
“[E]ducation on symptom recognition and physician training on new technologies may facilitate timely diagnoses and improve patient outcomes.”– Juday, et al., 2024
Since some new therapies work by slowing disease progression in the earliest stages of Alzheimer’s (and the prevalence of the condition is expected to double in the US by 2050), effective care for patients could hinge on timely diagnoses. Yet, missed and delayed diagnoses persist, a problem that is particularly acute among patients belonging to racial and ethnic minority groups.
One step toward mitigating disparities in Alzheimer’s care is a better understanding of how patients are diagnosed and treated at the beginning stages of their disease. To that end, we studied testing, referral, and treatment patterns among patients with early Alzheimer’s in community-based practices across the US. Below, we summarize two of our findings.
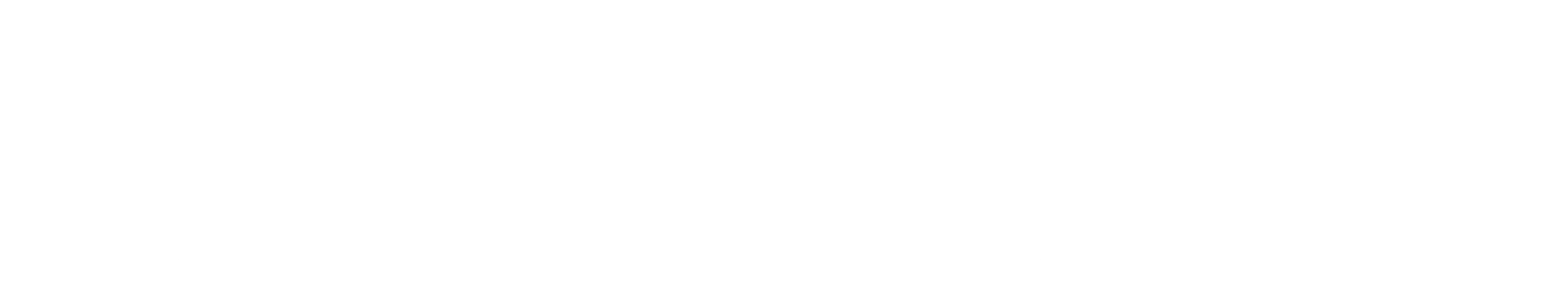
Determining Rates of Neurocognitive Assessments
Among all patients studied, we found that 16.1% did not receive any neurocognitive assessments (such as the Mini-Mental State Examination, Clock Drawing Test, or the Montreal Cognitive Assessment) in connection with their care. Additionally, non-white patients were less likely to receive neurocognitive assessments, as compared to white patients.
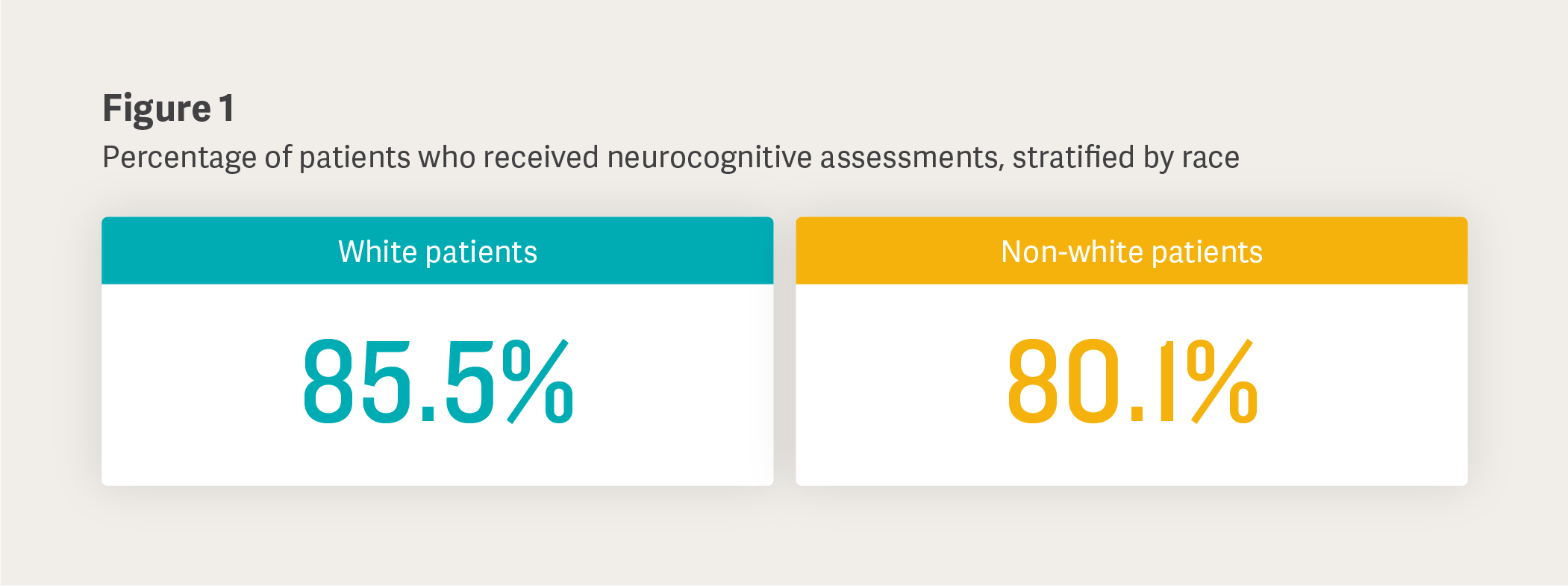
Evaluating Who Undergoes Imaging and Biomarker Tests
In our research, we found that 23.7% of patients did not receive a structural imaging or an Alzheimer’s disease–specific biomarker test. The administration of such tests was especially uncommon among patients from rural areas, as compared to those in urban or suburban settings.
Conclusion
We suggest that programs that shorten the time to diagnosis through appropriate health care provider referrals and the use of certain diagnostics may help reduce the time to detection and improve the treatment of early Alzheimer’s across sociodemographic groups. As diagnostic and treatment landscapes evolve, further research will be needed to determine standard diagnostic practices. By identifying disparities in the diagnostic process as it exists today, we aspire to close gaps in care for patients with Alzheimer’s and reduce the overall burden of the disease.
Keith Betts, Managing Principal
Ashley Holub, AssociateAdapted from “Real-world diagnostic, referral, and treatment patterns in early Alzheimer's disease among community-based practices in the United States,” Journal of Alzheimer’s Disease (2024), coauthored by Timothy R. Juday, Richard Batrla, and Feride H. Frech (Eisai); Soeren Mattke (University of Southern California); Ashley Holub and Keith Betts (Analysis Group); Sophie A. Kitchen (Alexion); Hongjiao Liu (University of Cambridge); and Ara S. Khachaturian (Prevent Alzheimer's Disease 2020).
This feature was published in June 2025.