-
In-Office Dispensing Could Improve Treatment Access and Clinical Outcomes for Nonmetastatic Castration-Resistant Prostate Cancer Patients
The use of existing services could reduce disparities in access to novel therapies and improve outcomes among patients with nonmetastatic castration-resistant prostate cancer (nmCRPC).
Since 2010, the distribution of next-generation oral anticancer medications has been increasingly handled through pharmaceutical services that are integrated into clinical practices. Known as in-office dispensing, these services have been shown to positively impact access to some interventional therapies among patients with prostate cancer.
“[T]his study suggests that continuity of care and the utilization of [in-office dispensing] services for patients receiving [next-generation treatments] may be critical to maximizing the benefits of oral anti-cancer therapy, thereby leading to improved clinical outcomes.”– Burbage, et al., 2024
Despite this, no prior literature has evaluated how in-office dispensing services may influence disease progression and clinical surveillance patterns among patients with nmCRPC specifically.
Additionally, other studies have shown that Black patients diagnosed with prostate cancer experience higher rates of mortality related to their disease and are less likely to be prescribed next-generation treatments as part of their care, as compared to the overall population of prostate cancer patients. Since prior studies report that survival outcomes among Black patients with prostate cancer are similar to those of the overall population when those patients are provided the same therapies, in-office dispensing services may help bridge a gap in access to life-saving treatments.
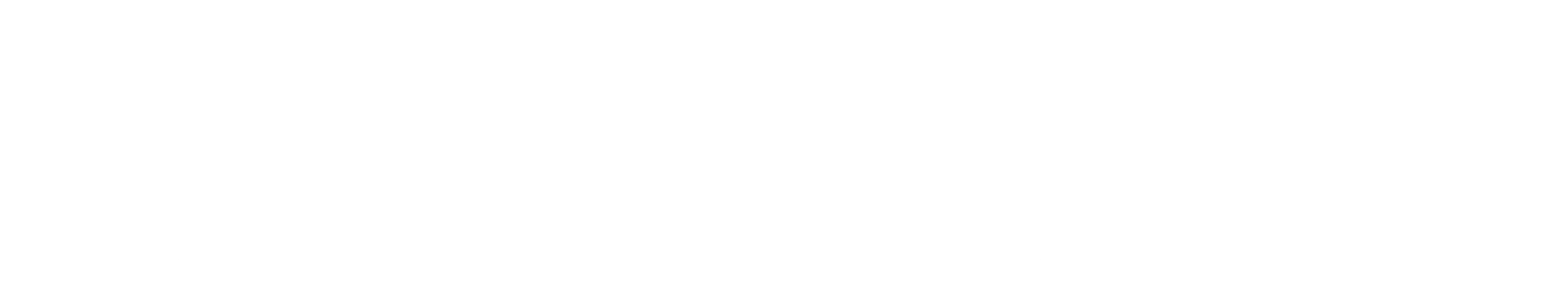
In our study, we divided 3,300 patients with nmCRPC who were prescribed next-generation treatments into three mutually exclusive cohorts: those who filled prescriptions for next-generation treatments using in-office dispensing services (IOD+), those who had access to in-office dispensing but chose not to use it (IOD-), and those who did not have access to in-office dispensing (non-IOD). To understand whether observations were consistent among Black patients with nmCRPC, we then restricted our analysis to focus on surveillance and outcomes for those patients. Below, we summarize two of our key findings.
Positive Impacts on the Overall Population Studied
Descriptively on average, we found that patients with nmCRPC who filled a prescription for a next-generation treatment using in-office dispensing services required fewer and less frequent bone scans, CT scans, and next-generation imaging than other patients. This could be indicative of an association between filling a prescription using in-office dispensing services and improved clinical outcomes.
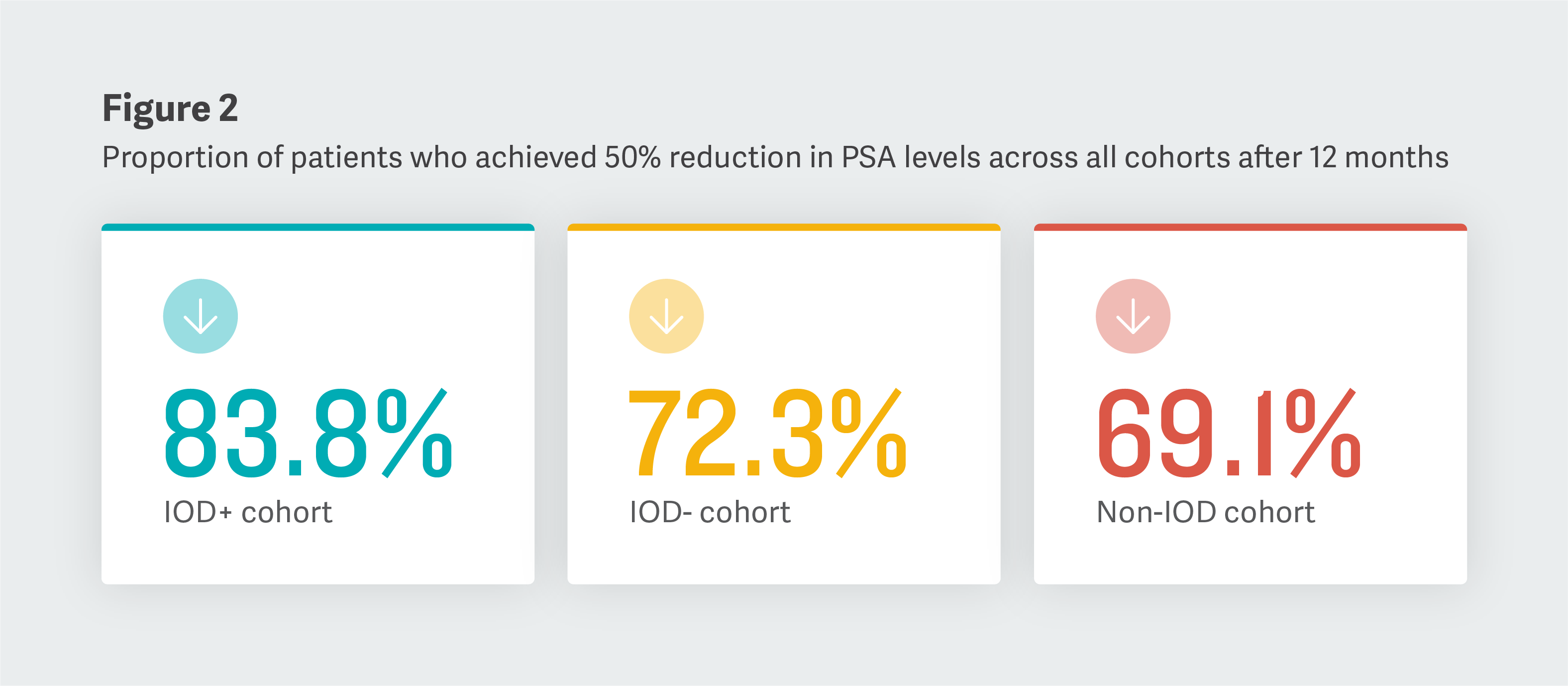
To further explore the impact of in-office dispensing services on nmCRPC patient care, we examined the percentages of patients who experienced significant declines in their baseline levels of a prostate cancer biomarker (prostate-specific antigen, or PSA) over time, across the cohorts studied.
Six months following initial treatment, we observed that the largest percentage of patients who experienced treatment response – defined as reductions in PSA levels – filled their prescriptions using in-office dispensing services. After a year, the differences that we observed between the cohorts that we studied followed a similar pattern.
Consistent Trends Observed Among a Restricted Population
Following our study of the overall population, we separately restricted our analysis to particularly evaluate how in-office dispensing services affect surveillance and PSA outcomes for Black patients with nmCRPC. The trends that we observed in our subgroup analysis were consistent with those of the overall analysis.
Since the overall differences that we observed were reflected among the subgroup of Black patients that we studied, the use of in-office dispensing services may be linked to increased access to next-generation treatments and improved outcomes among Black patients. Additional investigation will likely be needed to draw any comparative conclusions between subgroups of patients.
Conclusion
Descriptively, our study found that greater proportions of patients using in-office dispensing services can achieve better outcomes relative to those who may not use or may not have access to those services, irrespective of the race of those patients. Further research controlling for differences in baseline characteristics and examining longer-term outcomes is needed to understand how in-office dispensing services could impact the quality of oncology patient care. ■
Patrick Lefebvre, Managing Principal
Dominic Pilon, Vice President
Carmine Rossi, Manager
Frederic Kinkead, AssociateAdapted from “PSA Outcomes and Clinical Surveillance Among Patients With Nonmetastatic Castration-Resistant Prostate Cancer Treated With a Next-Generation Androgen Receptor Inhibitor in Urology Practices With or Without In-Office Dispensing,” Journal of Clinical Pathways (2024), coauthored by Sabree C. Burbage (Johnson & Johnson Innovative Medicine); Dexter Waters (Johnson & Johnson Innovative Medicine); Carmine Rossi (Analysis Group); Frederic Kinkead (Analysis Group); Erik Muser (Johnson & Johnson Innovative Medicine); Lorie Ellis (Johnson & Johnson Innovative Medicine); Patrick Lefebvre (Analysis Group); and Dominic Pilon (Analysis Group).
This feature was published in November 2024.