-
Measuring Treatment and Overall Survival Differences Between White and Black Patients with Metastatic Castration-Sensitive Prostate Cancer
Novel treatment options could help raise overall survival for a particular form of cancer, but troubling gaps in usage persist.
Over the last decade, treatment guidelines for prostate cancer have evolved. Promising clinical trial evidence has shown prolonged overall survival among patients with prostate cancer who have received treatment intensification (TI) – that is, combining either a novel hormonal therapy or a chemotherapy with androgen deprivation therapy. As a result, TI is now recommended for patients with prostate cancer, including those with metastatic castration-sensitive prostate cancer (mCSPC), which is marked by the spread of cancer cells from the prostate to other areas of the body.
“[T]hese data may signal that urgent action is needed to make mCSPC treatment more guideline-adherent.”– George, et al., 2024
Patients at this stage of cancer are still sensitive to, and therefore able to be treated with, androgen deprivation therapy. Clinical trials show that overall survival in this population could be improved with TI. However, those trials included very few Black patients.
In our study, we examined real-world data about the use of TI and overall survival among Black versus white patients with mCSPC in Medicare and Veterans Health Administration (VHA) populations. Below, we summarize some of our key findings.
Slow Uptake of TI
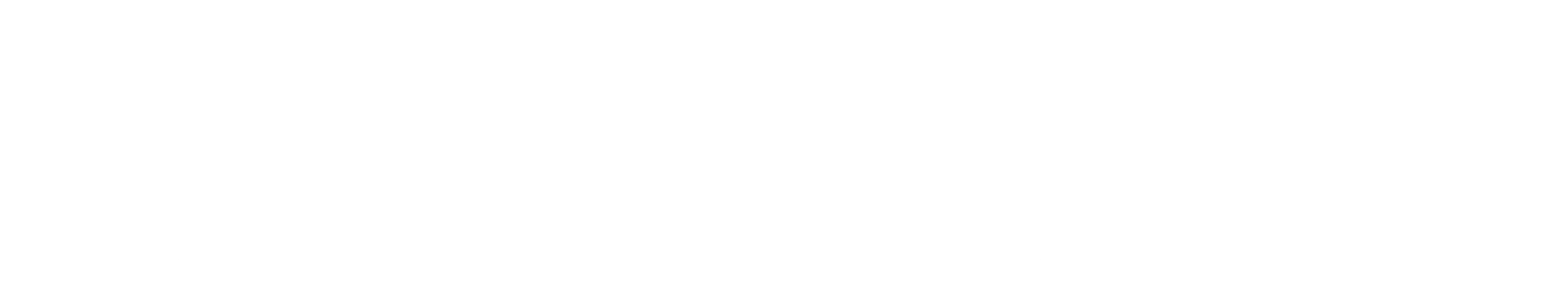
TI was underutilized among the overall population of patients with mCSPC that we studied. Even in the most recent years of data available, more than two-thirds of all patients did not receive US Food and Drug Administration (FDA)-approved and guideline-recommended TI for their condition. Additionally, Black patients were significantly less likely than white patients to receive TI for mCSPC, regardless of whether they were enrolled in Medicare (32% less likely) or the VHA (25% less likely).
Impact on Overall Survival
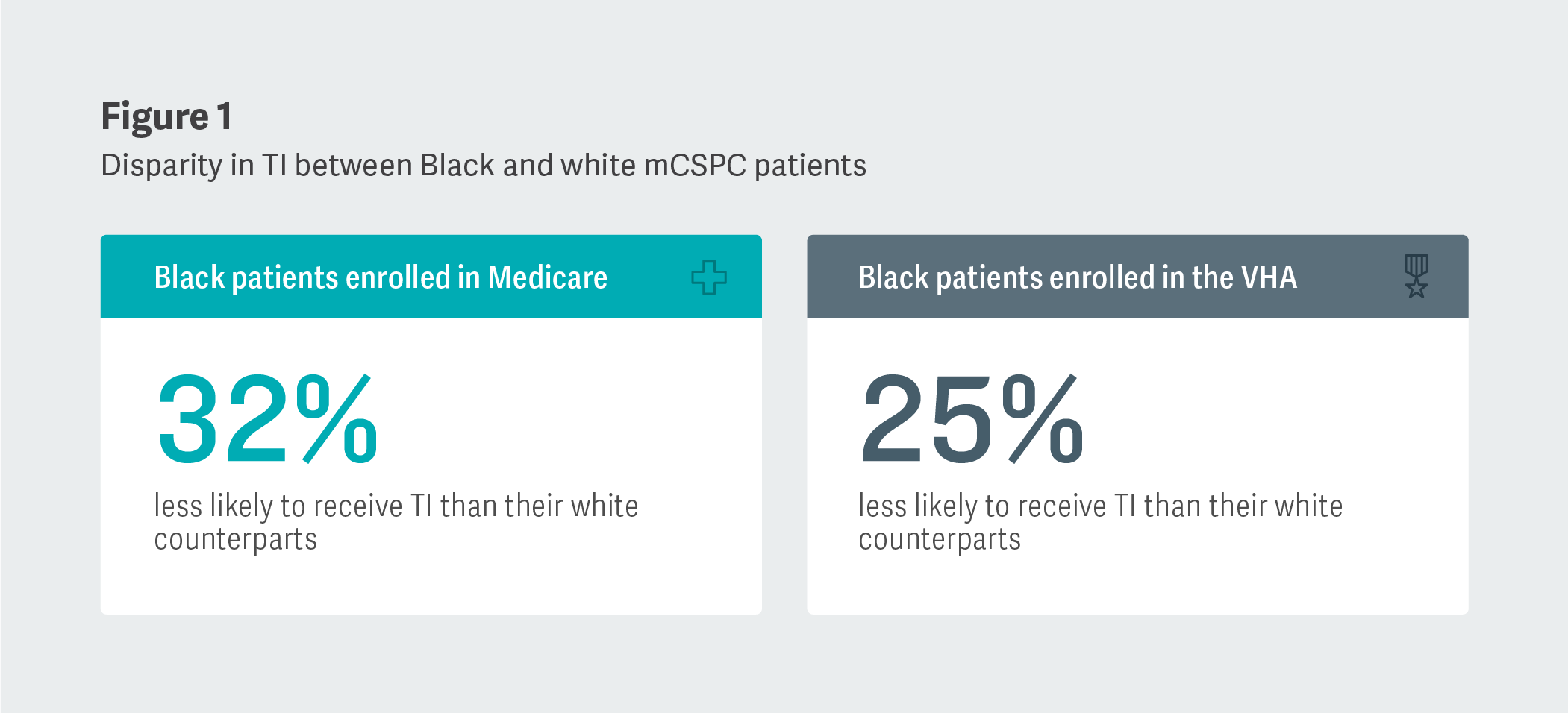
Black patients were also shown to experience a higher risk of death (20% higher) than white patients with mCSPC in the Medicare population. However, Black and white patients had a similar risk of death in the VHA population. In addition, Medicare patients who were Medicaid-enrolled were less likely to receive TI and 50% more likely to die than those not enrolled in Medicaid (regardless of race), which suggests that poverty, in addition to race, is associated with quality of care and outcomes.
“If emerging disparities in TI in mCSPC are not addressed aggressively, selective increased use of TI in [w]hite patients, including treatment combinations, may further increase disparities in outcomes.”– George, et al., 2024
Conclusion
Our study contains strong indications that disparities by race and socioeconomic status exist in mCSPC treatment. Further research in this area is needed to uncover the factors driving these disparities and to suggest ways of overcoming them. We hope that this study will serve as a piece of real-world evidence that may help health care providers in their assessment and treatment of patients with mCSPC and eventually contribute to better overall survival outcomes. ■
“[I]t is concerning that treatment disparities and potentially worse survival outcomes are emerging in mCSPC when life-prolonging treatments are available and established as the standard of care.”– George, et al., 2024
Hongbo Yang, Managing Principal
Wei Gao, Vice President
Wei Song, ManagerAdapted from “Emerging racial disparities among Medicare beneficiaries and Veterans with metastatic castration-sensitive prostate cancer,” Prostate Cancer and Prostatic Diseases (2024), coauthored by Daniel J. George and Rhonda L. Bitting (Duke Cancer Institute); Neeraj Agarwal (University of Utah); Krishnan Ramaswamy, David Russell, Rickard Sandin, Birol Emir, and Agnes Hong (Pfizer); Zachary Klaassen (Georgia Cancer Center); Hongbo Yang, Wei Song, and Wei Gao (Analysis Group); Yilu Lin (Tulane University); and Stephen J. Freedland (Durham VA Medical Center).
This feature was published in June 2024.